Abstract

Introduction Multiple myeloma (MM) is disproportionately a disease of older adults, with a median age at diagnosis of 69. Prior single-center studies and therapeutic trials have demonstrated that aging-related functional impairments in activities of daily living (ADLs - e.g., bathing, toileting) are common among this population and predict treatment intolerance, healthcare utilization, and mortality. However, the prevalence and impact of functional impairments among broader, more generalizable populations of older adults with MM is less well understood.
Methods We utilized cancer registry data from the Surveillance, Epidemiology, and End Results (SEER) program linked with Medicare enrollment and claims data from 2008-2019 and the Outcome and Assessment Information Set (OASIS) from 2008-2018 to construct a retrospective cohort of adults aged ≥66 diagnosed with MM between 2009 and 2017. OASIS data capture functional assessments for Medicare beneficiaries who are home health care recipients (HHRs). Individuals were deemed home health recipients if they had at least one OASIS assessment in the 12 months prior to MM diagnosis (inclusive of month of diagnosis).
The primary exposures were (1) receipt of home health services prior to MM diagnosis and (2), degree of functional disability, a composite score derived from individual items related to ADLs contained in the OASIS data for HHRs and categorized by tertile as mild (composite score 0-11), moderate (12-17) or severe disability (18-40). The primary outcome was overall mortality within 5 years from diagnosis. Associations between primary exposures and outcomes were assessed via cumulative risk ratios (RRs) at 6, 12, and 36 months from diagnosis, with bootstrapped 95% confidence intervals. The association between receipt of any home health services and mortality was unadjusted; the association between degree of functional disability and mortality among those receiving home health services was adjusted for age, sex, race, and SEER region via inverse probability weighting.
Results Among 41,635 beneficiaries with MM, 6,850 (16.4%) received home health services and had an OASIS assessment in the year prior to diagnosis. When compared to non-recipients, HHRs were older (38.6% in highest quartile vs 22.5%), more likely to be non-Hispanic Black (19.9%% vs 17.2%), and more likely to live in counties with greater rates of poverty (25.2% in highest quartile vs 21.7%). HHRs had similar rates of rural residence (10.5% vs 10.8%).
Among HHRs, 79% required assistance with at least one ADL. Median number of activities with which HHRs required assistance was 3 (range 0-7).
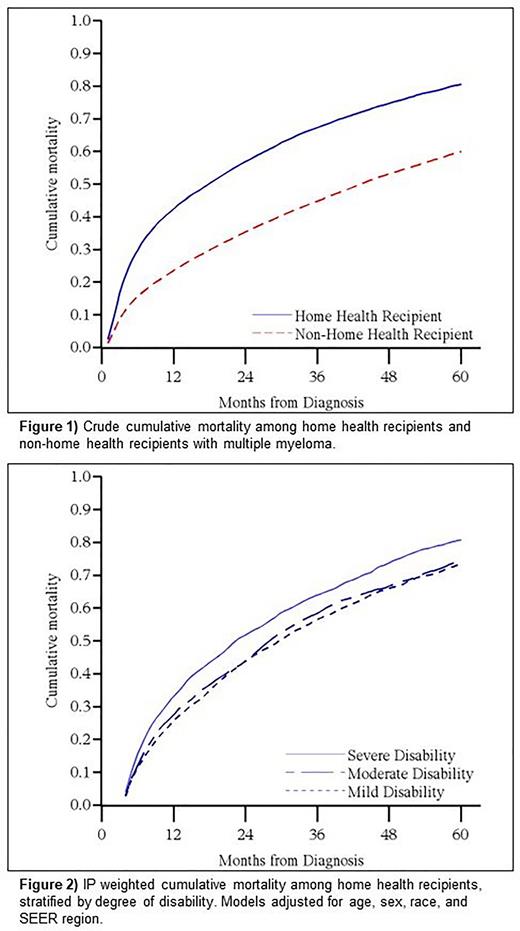
HHRs had higher all-cause mortality at all assessed time points compared to non-HHRs with MM (Figure 1); RRs were 1.91 (95% CI 1.83-1.99) at 6 months from diagnosis, 1.80 (1.74-1.86) at 12 months, and 1.50 at 36 months (1.47-1.53).
Among HHRs, mortality was higher among those with severe functional disabilities compared to those with mild disability; RR for the severe versus mild disability groups was 1.38 (1.17-1.62) at 6 months, 1.29 (1.17-1.43) at 12 months, and 1.13 (1.08-1.19) at 36 months. In contrast, those with mild and moderate degrees of disability had similar survival (Figure 2), with non-significant differences in mortality at all assessed time points.
Conclusions In this large nationwide study of older adults with MM, we describe the association between physical disability/activity dependence and 5-year mortality. These findings corroborate results of prior, smaller studies based on data from academic centers or therapeutic clinical trials. Our study is novel for its use of a large, diverse, and generalizable data source and the recent linkage with OASIS records.
In this cohort, home health recipients had higher 5-year mortality compared to non-home health recipients. Additionally, mortality was most profoundly impacted among those with severe disabilities. In contrast, those with moderate degrees of disability had mortality rates that did not differ significantly from those individuals with mild disability. This moderate disability group, who had a median survival measured in years, may be at risk for undertreatment if their prognosis is underestimated. Future research will characterize the impact of physical disability on MM therapy receipt among this population.
Disclosures
Jensen:Conquer Cancer Foundation: Research Funding. Leblanc:GSK: Membership on an entity's Board of Directors or advisory committees. Reeder-Hayes:Pfizer Global Medical Foundation: Research Funding; American Cancer Society: Research Funding; Conquer Cancer Foundation: Research Funding; Susan G Komen Foundation: Research Funding.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal